Services
- Home
- Mental Health Services
- Who We Treat
- How We Treat
- Patients & Visitors
- About
close

Parents, grandparents, and other caregivers often are the first to notice behaviors with the young boy or girl under their care that give them small pauses for concern. They may brush them off or be hesitant to fully recognize signs of attention-deficit/ hyperactivity disorder (ADHD), these symptoms are often mistaken for Autism. After all, aren’t children supposed to be full of energy or seem lost in the wonder of their thoughts?
It’s not hurting anyone so why push it, some might say. Then the school year starts and the notes start coming home in their class folder. These notes chronicle classroom behaviors or quality of work that are becoming worrisome to their teacher and often lead to a parent/teacher conference. Little Jackson seems to enjoy getting up from his chair and wandering the classroom in the middle of an instruction. Little Zoe seems to fidget on the carpet during reading time and is unable to focus on completing her assignments in art class.
Not only are these incidents affecting their child’s school performance, but they are causing distractions to other students and making it difficult for the teacher to handle everyone’s needs adequately. Filled with trepidation beforehand, parents often leave these meetings worried, with the teacher urging them to have little Jackson or Zoe be tested for ADHD.
The teacher does offer this beacon of hope: if Jackson or Zoe does meet the criteria for an ADHD diagnosis, the school can then provide resources that will support everyone’s needs, including an educational aide assigned to help keep distractions to a minimum in class and to focus on tasks. In addition, the student is eligible for special instruction that will help teach them to manage their ADHD behaviors as they grow older, and they can take tests with time allowances added or in a quiet environment.
When a parent learns their child has been diagnosed with ADHD it can bring on a variety of emotions. You may feel some relief to have a name assigned to your child’s condition, quickly replaced by questions related to what caused it.
ADHD is a neurodevelopmental disorder, meaning it stems from a problem with brain development. When researching risks and causes behind the disorder there are many unknowns, but scientific research points to genetics playing a potential role. Studies have linked genetics in studies of twins as “high heritability” and “moderate broad heritability” in non-twin children, adolescents, and adults. There is also a consideration that ADHD occurring in childhood can last into adulthood.
Oftentimes, parents or grandparents may limit sweets or instruct babysitters to do likewise for children that tend to be behaving wildly. Generally, that is good advice, but high sugar intake is not the cause of ADHD. What it can do, along with caffeine, is contribute to the symptoms.
The same can be said for watching too much television, and misguided parenting in the heat of the moment. Other external contributors include having a noisy or chaotic home, and even poverty may play a role. But at the root is the neurological development factor.
Genetics aside, the Centers for Disease Control (CDC) said researchers continue to study other possible causes of ADHD including
In general, parents or a teacher notice overall impulsive behavior, difficulty focusing, and hyperactivity. The child, teen, or adult may struggle to act in an age-appropriate manner or use good judgment.
The CDC references these main symptoms, but they are part of a longer list of specific areas in which a child must meet a minimum of behaviors to meet the diagnostic criteria:

A psychologist, psychiatrist, or primary care doctor are all qualified to diagnose ADHD with input from parents, teachers, and other adults who supervise the child regularly and can provide valuable input regarding behavior.
In addition, they will look to meet at least six of nine indicators of inattention and six of nine indicators of hyperactivity and impulsivity. Four other conditions must all be present as well regarding symptoms appearing before age 12, behaviors occurring in multiple environments, symptoms interfering with activities, and other possible causes are ruled out.
Boys are typically three times as likely to be diagnosed than girls with ADHD, but that is most likely related to boys’ symptoms being more external whereas girls’ symptoms are more internal and less likely to be diagnosed. In essence, they may seem dreamlike and have trouble focusing but may not be as likely to cause the noisy disruptions a boy might. Both can still suffer long-term issues with schoolwork and meeting deadlines as the disorder affects their daily life.
One 2013 study of 37 females and 43 males ages 8-17 noted girls more frequently self-reported experiencing anxiety symptoms, and parents noticed that their boys gravitated more toward “rule-breaking.”
The World Health Organization World Mental Health Surveys examined the issue among 20 countries globally in 2017 by asking adults ages 18-44 to reflect upon their childhood and noted the United States scored the highest frequency of childhood ADHD at 8.1%, nearly double that of the second-closest country, France at 4.7%. The remaining countries scored between 0.1% for Iraq and 3.2% for Northern Ireland.

As your child grows older, and for adults who are just realizing the possible cause of behaviors they may have had since childhood or developed more recently, the criteria for ADHD diagnosis are somewhat different. Instead of meeting six symptoms, adults and adolescents age 17 years or older, only need to display five symptoms.
In addition, they might not have issues with wandering a classroom, but oftentimes feel restless or full of activity that may overwhelm others.
There are three presentations for ADHD:
You may see your child’s symptoms change as he or she ages, and their presentation may change.
“Between 5 percent and 75 percent of children with ADHD can continue to have the disorder into adulthood,” said Dr. Arunima Roy, MBBS, Ph.D., and research fellow at the Royal’s Institute of Mental Health Research, University of Ottawa.
Dr. Roy was the lead author of a 2019 study examining the effects of childhood and adult ADHD on risk factors for motor vehicle accidents. In addition to a 1.45-times-higher risk of accidents, ADHD can also impact a person with “occupational performance, educational attainment, emotional functioning, substance use, and justice involvement,” she said.
“Extant research shows that ADHD is associated with more traffic violations, speeding violations, license suspensions, and risky driving behaviors. The likelihood of risky driving behavior increases with persistence of childhood ADHD symptoms into adulthood. Prior research from our group as well as by others also shows that, aside from driving behaviors, a persistence of ADHD into adulthood can impair functioning in other domains.”
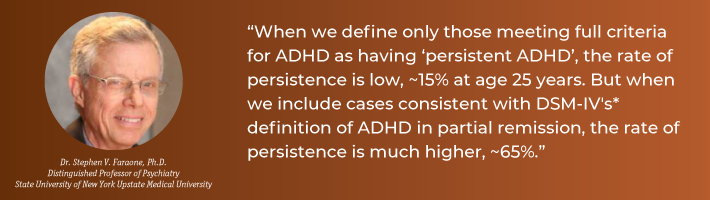
Yet another study said the commonality of continuing ADHD into adulthood occurs between 50-65%, depending on “how one defines persistent.”
“When we define only those meeting full criteria for ADHD as having ‘persistent ADHD’, the rate of persistence is low, ~15% at age 25 years. But when we include cases consistent with DSM-IV's* definition of ADHD in partial remission, the rate of persistence is much higher, ~65%,” according to lead author Dr. Stephen V. Faraone, distinguished professor of psychiatry, State University of New York Upstate Medical University.
Learning to live with and manage attention-deficit/hyperactivity disorder is especially important as children grow into young adults during their adolescent years. Let’s face it, the teenage years can be tough enough!
Organizational tools can be helpful as well and adapted as the child takes more ownership with age and shows improvements.
As mentioned earlier, by receiving the diagnosis, your child’s school will be better positioned to assist with educational remedies. Intervening in disruptive behaviors early, before they escalate, can help the child see the connection between what's happening at school and what they were taught with their parents for behavior management. This can help with school performance and getting along with other classmates.
Our Adolescent Psychiatry Program is designed for ages 12-17; this age group makes up half of the six million people diagnosed with ADHD. Identifying school support services, behavioral therapy, and possibly medication can all be considered for treatment plans for ADHD.
If you are looking for teen therapy in Houston to help manage ADHD or other mental issues, we encourage you to reach out to SUN Behavioral Houston. In addition to our Adolescent Psychiatry Program for teens, we also offer a Children Program for ages 6-12, both to help build strong futures. Our values are the core of our mission to provide mental health services for our patients and their loved ones. Call us today at (713) 796-2273.
Are You Born With ADHD, or Can It Develop?
You may have a genetic predisposition for developing ADHD, but symptoms are not usually recognized as disruptive or concerning until patterns are repeated over time in early childhood.
What Causes ADHD in Children?
There are indications linking genetics to ADHD, but other possible factors include environmental toxin exposures such as lead during pregnancy or at a young age, alcohol and tobacco use during pregnancy, premature delivery, or low birth rate.